The State of Young Physicians


In this study, our goal was to capture the values and goals of young physicians and explore the factors they believe will influence the delivery of healthcare in 2035. To achieve this, in July of 2024, we hosted conversations with 8 young physicians aged 21-35, followed by an engagement of 1,018 young physicians in a nationwide survey.

1. Driven by Personal Connections
At the core of young physician’s values is the ability to help and heal. This drive not only impacts how they feel about medicine today, but how they want to practice in the future. Remove the personal connection from the doctor, and you remove the heart out of healthcare.
2. Value-Based Medicine for Value-Based Care
Young physicians prioritize working for healthcare organizations whose values align with their own from a clinical, cultural and ethical perspective. These physicians expect healthcare institutions to demonstrate a strong commitment to core values that align with their beliefs around equity, inclusivity, and work-life balance — or else miss the mark on realizing value-based care.
3. The Vast, Two-Way Trust Gap
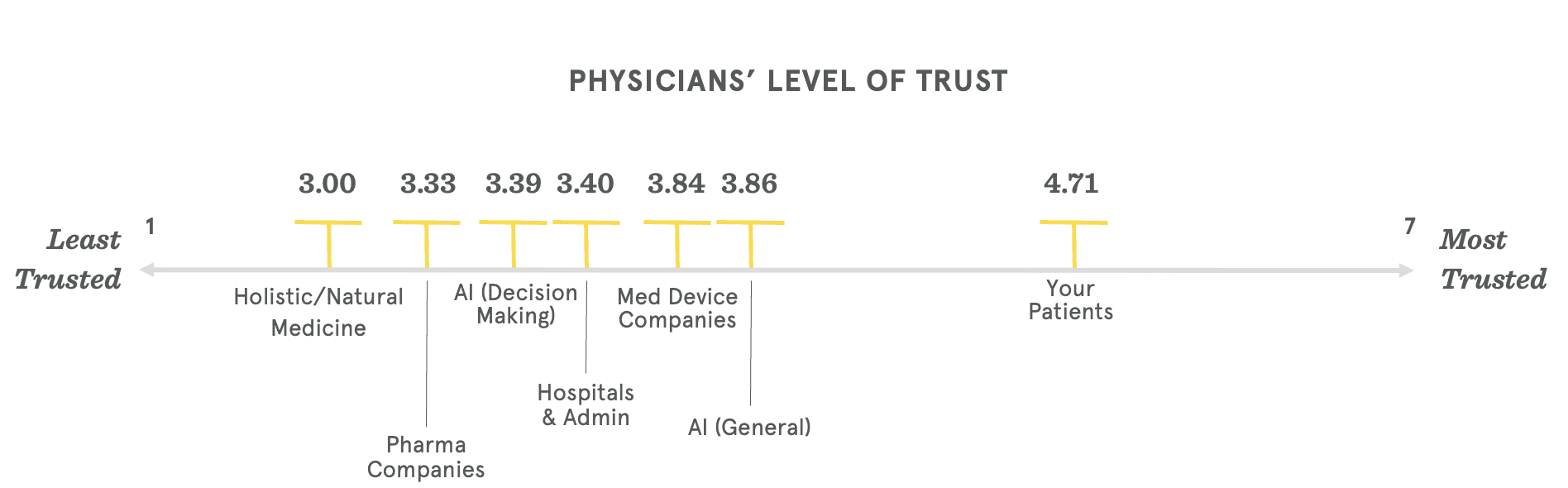
Trust is significantly eroding between both patients and physicians. In 2035, young physicians project misinformation to be a major challenge in their relationships with patients. Well over half (59%) of young physicians predict that in 2035, patients will be less trusting of their doctors.
4. The Future of Care is Treating Upstream
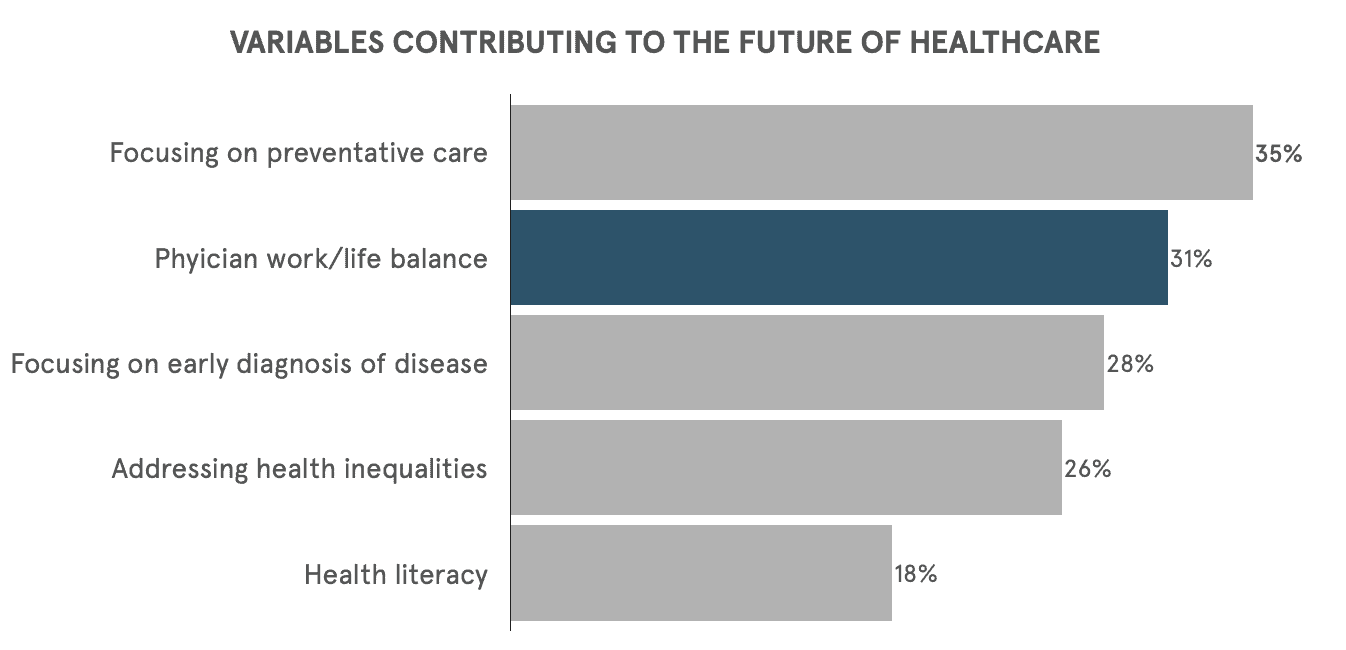
Young physicians feel strongly about the impact of early interventions (including preventative measures, precision medicine, and diagnostics), considering them to be key drivers that will make the most positive impact on the delivery of care in 2035. For young physicians, the top three variables for contributing to the delivery of healthcare are: (1) preventative care, (2) early diagnosis, and (3) addressing health inequalities.
5. The Expected Role of AI as an Enabler
Our population of young physicians see immense value in integrating new technologies into their practice. Over three quarters of young physicians predict that AI will play an “assistant” role in their day-to-day practice.
6. Progressing Clinical Trial Development
Young physicians are increasingly interested in shaping the future of healthcare through involvement in clinical trials and collaboration with medical device and pharmaceutical companies. Doing so could address practical challenges and align with current medical practices and beliefs.
7. The Divergence and Diversity of Decision Making
Young physicians harbor reservations about the expanding roles of providers, as evidenced by a significant majority expressing concern over its potential negative impact by 2035. This calls to attention a need to address workforce shortages while maintaining rigorous standards and embracing technological advancements in medical education.
Meet the future of medicine — and our physicians of the future. Today, they span healthcare roles from attending physicians to residents to medical students. In 2035, they will be the decision-makers on the frontlines of realizing a patient-centric future that fulfills the true promise of value-based care via value-based medicine, prioritizes deep personal connections with their patients and leverages preventative care. This ambitious generation is poised to push the healthcare ecosystem to its highest potential — and they don’t expect anything less from their partner institutions to match their commitment and drive for excellence.
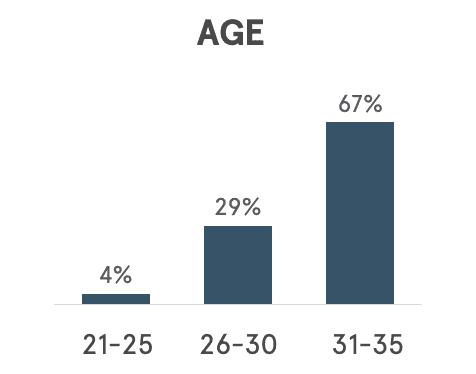
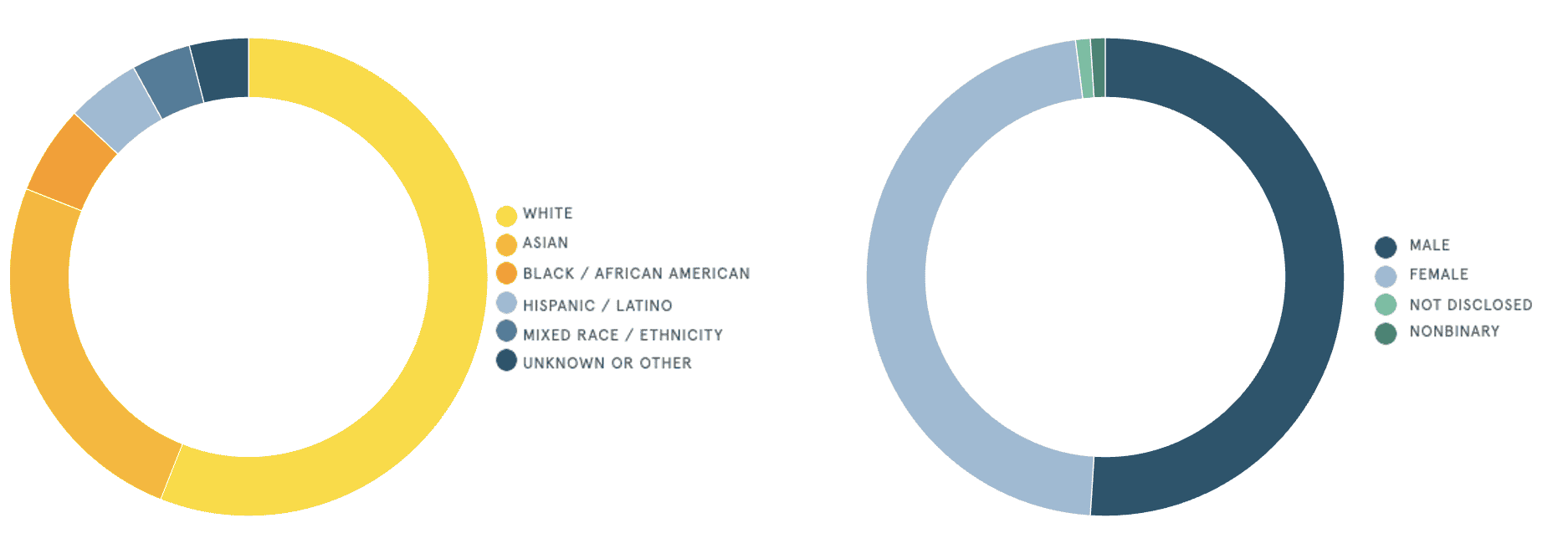
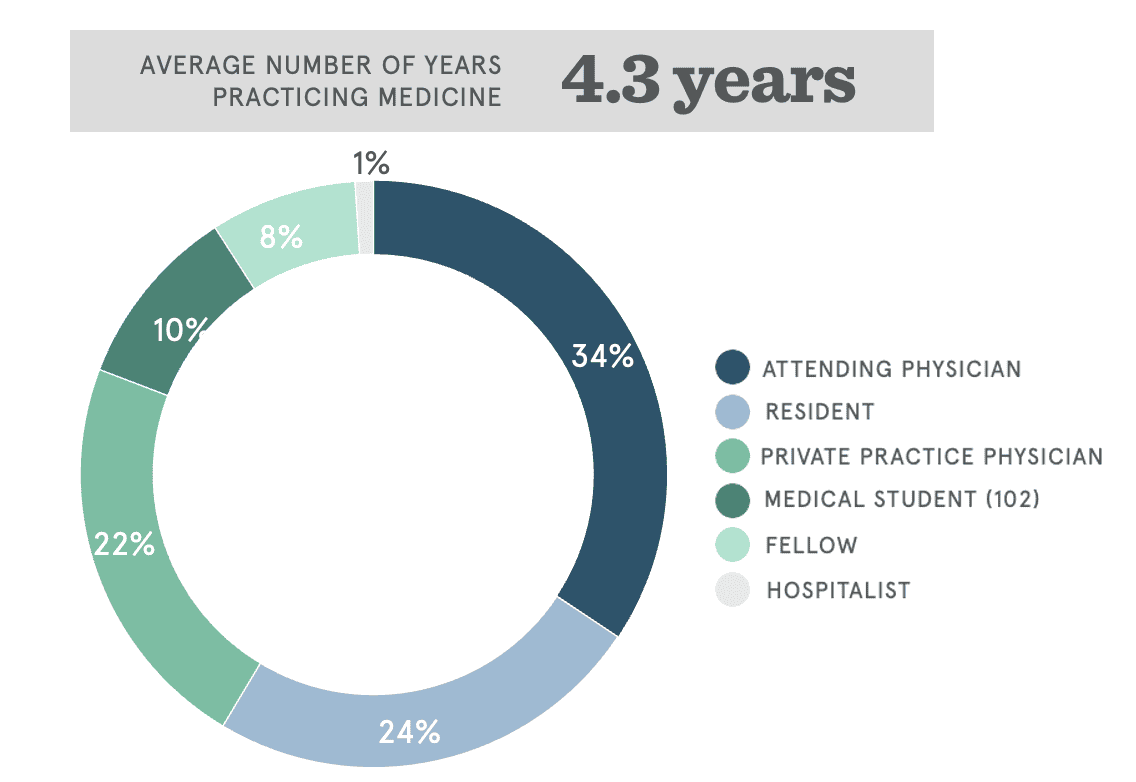
The young physicians in this study represent a sample of age, race, and gender that is consistent with the US global population. Our young physician cohort is comprised of 67% of physicians between the ages of 31-35, 29% between the ages of 26-30, and 4% between the ages of 21-25, with an average of 4.3 years of practicing medicine.
This report is informed by our cohort, 51% of whom identify as male, and 47% who identify as female. Just over half (56%) identify their race or ethnicity as white, another 25% Asian, and 6% black or African American.
These young physicians impact the healthcare ecosystem in various roles, practice settings, specialties, and the communities they serve. Over a third (34%) of respondents are attending physicians, another 24% are residents, and 22% are private practice physicians.
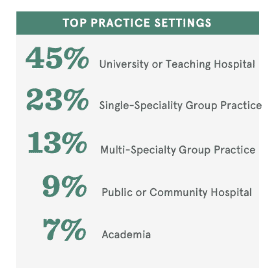
Over half (54%) of these physicians practice in an urban community, another 39% practice in a suburban community, and 7% practice in rural communities. The practice settings span a university or teaching hospital, where 45% of physicians practice, to single-specialty group practices (23%), multi-specialty group practices (13%).
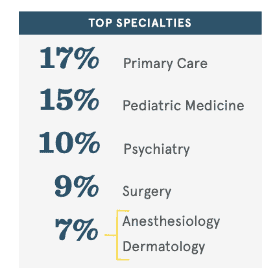
Nearly a fifth of respondents (17%) are board-certified or board-eligible to practice in primary care, another 15% in pediatric medicine, and 10% in psychiatry.
Young physicians are deeply motivated by the personal connections they make with their patients.
“Most of the people who become doctors for the human part of it … Most of us who decide to do the doctor part we like the science stuff a little bit, but we like the people stuff a lot more.” – Dr. Shirlene Obuobi, Cardiology Fellow – Chicago Medical Center
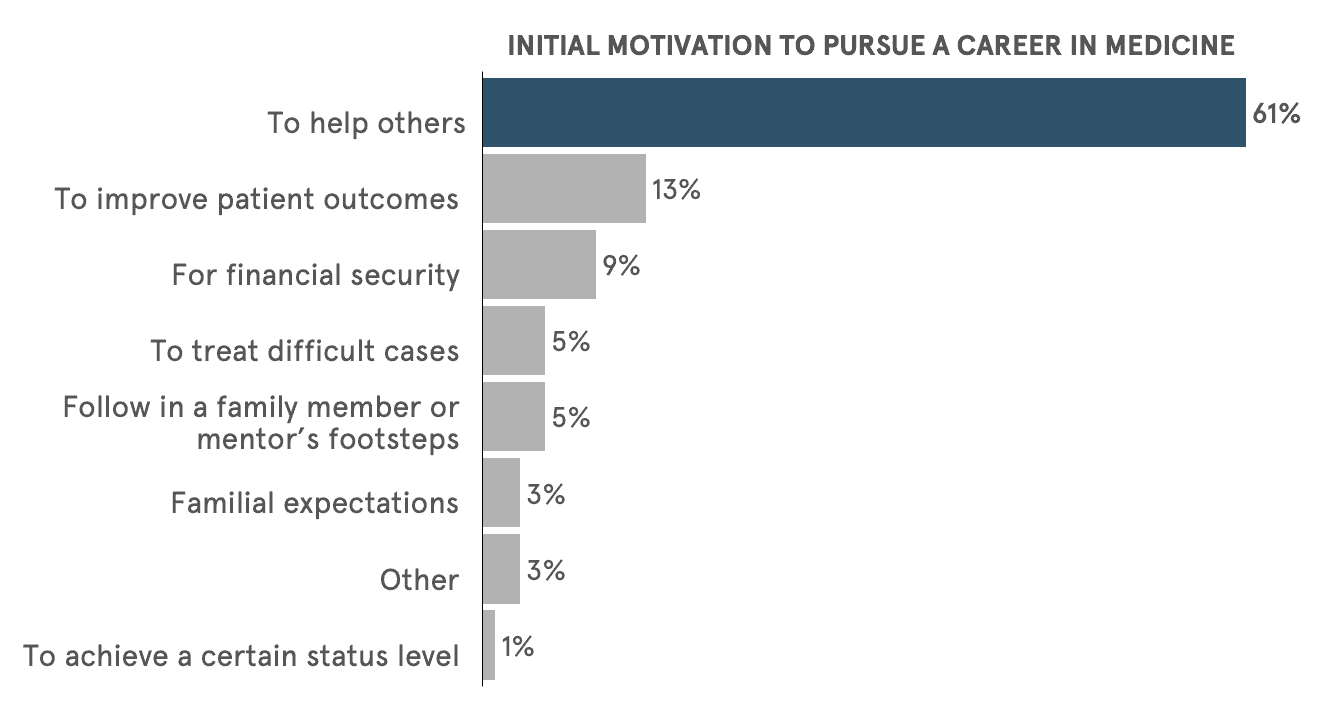
At the core of young physicians’ values is the desire to help and heal. Nearly three-quarters of young physicians indicate that their initial motivation to pursue a career in medicine was to help others and improve patient outcomes. That is in sharp contrast to what they are not motivated by: money and prestige. This sense of altruism reflects their intentions when they began their journey in medicine.
“I was in the hospital seeing a pediatric rheumatologist and I saw a bunch of children going by. One with their leg amputated and one going through chemo. And it hit me like a bolt of lightning. I was like, Oh, my gosh! This is what I need to do with my life. I just want to be able to pass that on and take care of other people.” – Medical Student
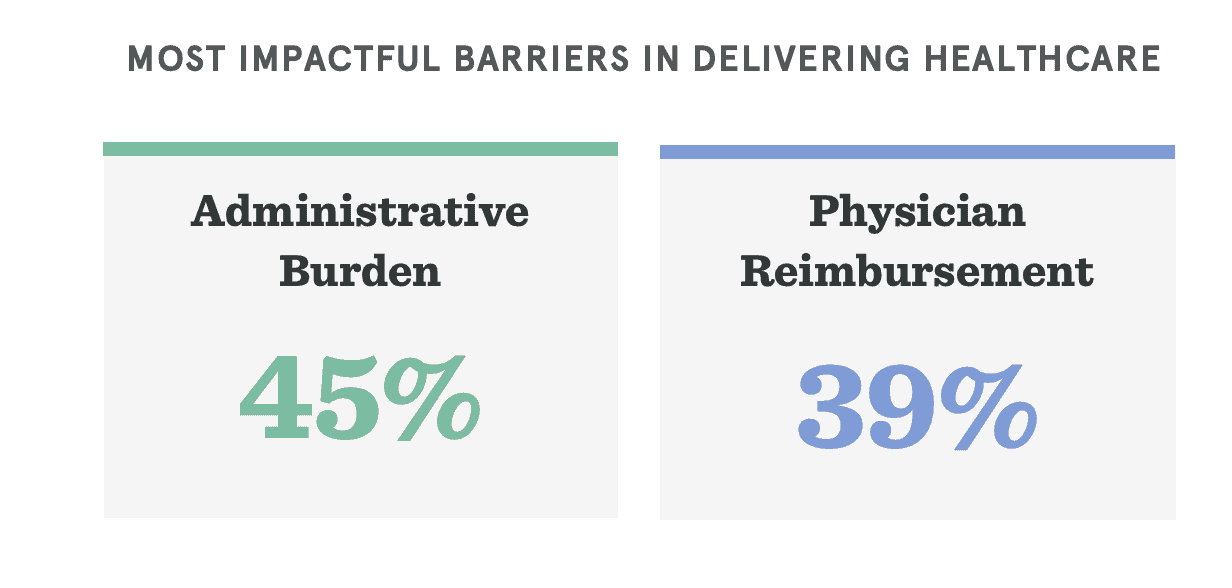
Administrative burden is a significant roadblock in physicians’ ability to deliver care, with 45% of respondents considering it to be a leading barrier to delivering care in 2035. Such an administrative tax stands in the way of physicians’ desire to develop connections that not only drive personal motivations, but lead to better health outcomes.
“If you get the processes that are necessary in a visit, it gives you more time to interact with your patient and get to know them. That’s what makes being a doctor worth it. The less time I can spend on the computer and the more time I can spend face-to-face with the patients makes me the happiest.” – Medical Student
“It is difficult getting through all the paperwork and administrative work. I spend too much time putting information into the computer and not being able to have enough facetime with my patients.” – Resident Physician, Pediatrics
Remove the personal connection from the doctor, and you remove the heart out of healthcare.
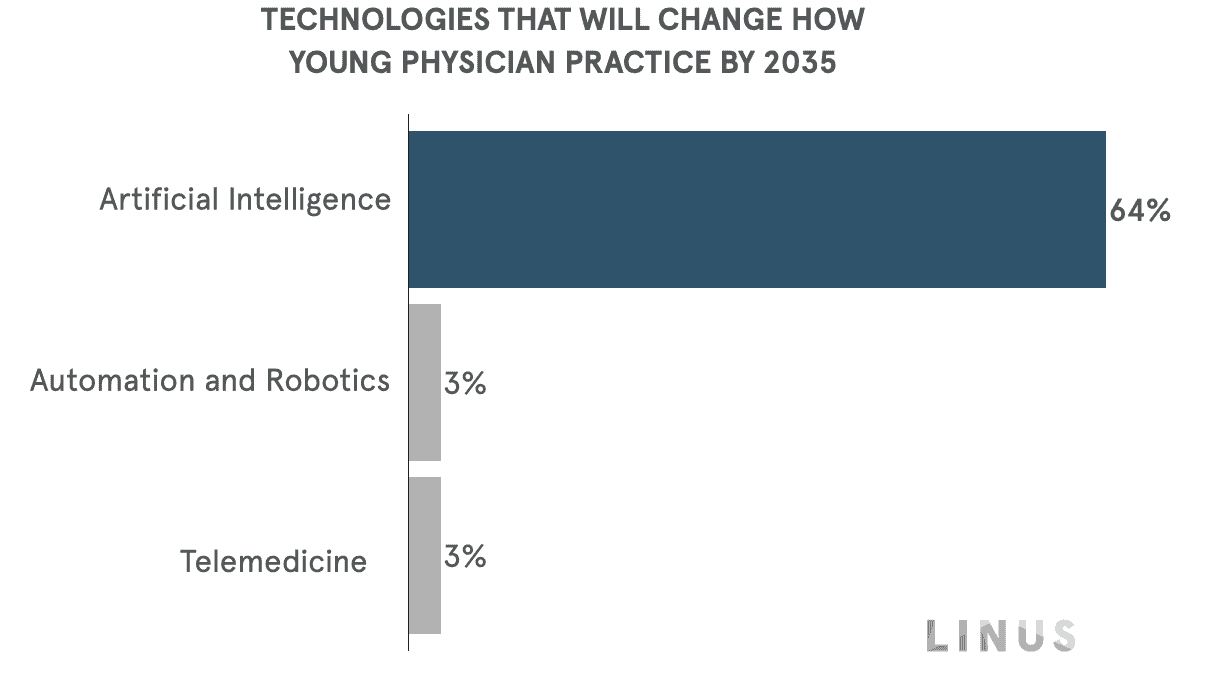
Nowhere is this more apparent than young physicians’ expectations in how artificial intelligence will change the way they practice. Around two-thirds of our respondents predict that integration of AI in the medical field will change how they engage patients. This is significantly higher (by 60 percentage points) than the second most mentioned technology: telemedicine.
“AI could have the power to change the documentation process, which is an extreme burden on physicians in all fields of medicine.“ – Fellow, Surgery
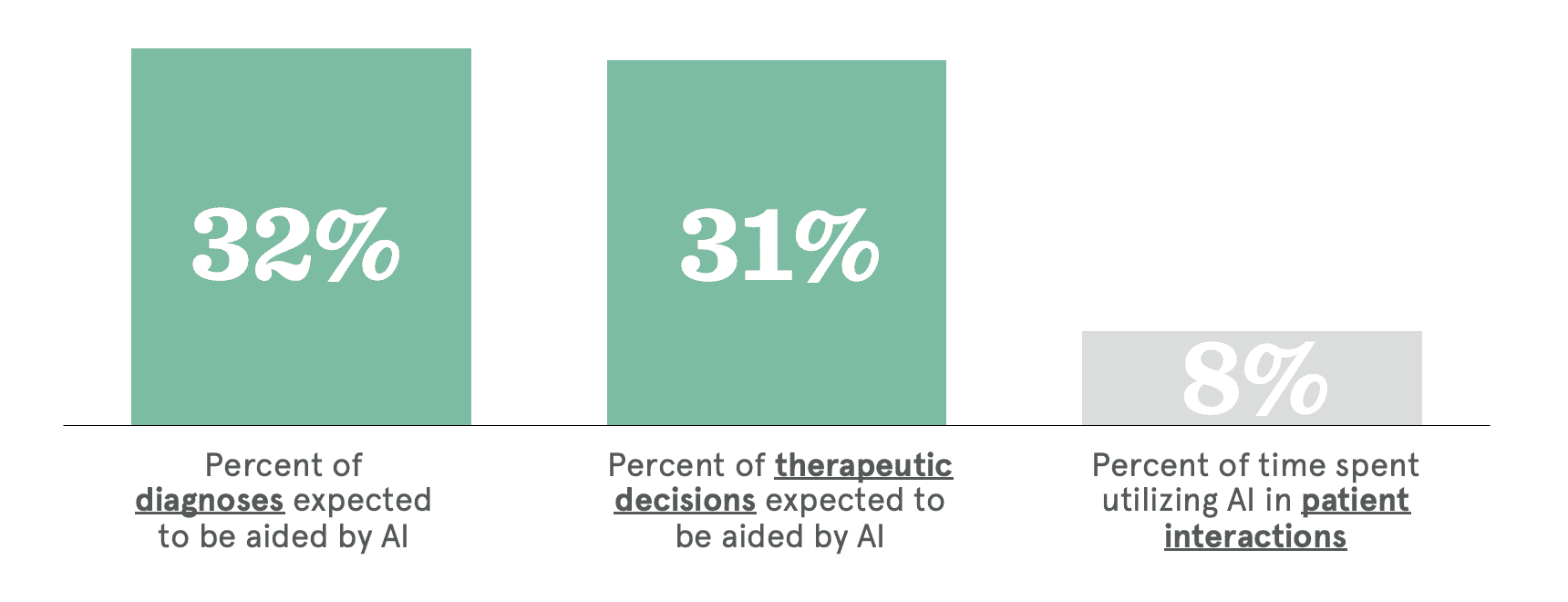
Specifically, young physicians see the potential of AI being effective in clinical decision-making, rather than in patient relationships. Young physicians predict by 2035, 32% of diagnoses and 31% of therapeutic decisions will likely be aided by AI, compared with a staggeringly low 8% of time spent using AI to interact with patients.
Personal connections are the key motivator for tomorrow’s physicians. If AI interferes or disrupts this primary source of patient interaction, then technology and administrative processes will contribute to further physician burnout, instead of fostering relationships.
Young physicians prioritize working for healthcare organizations whose values align with their own.
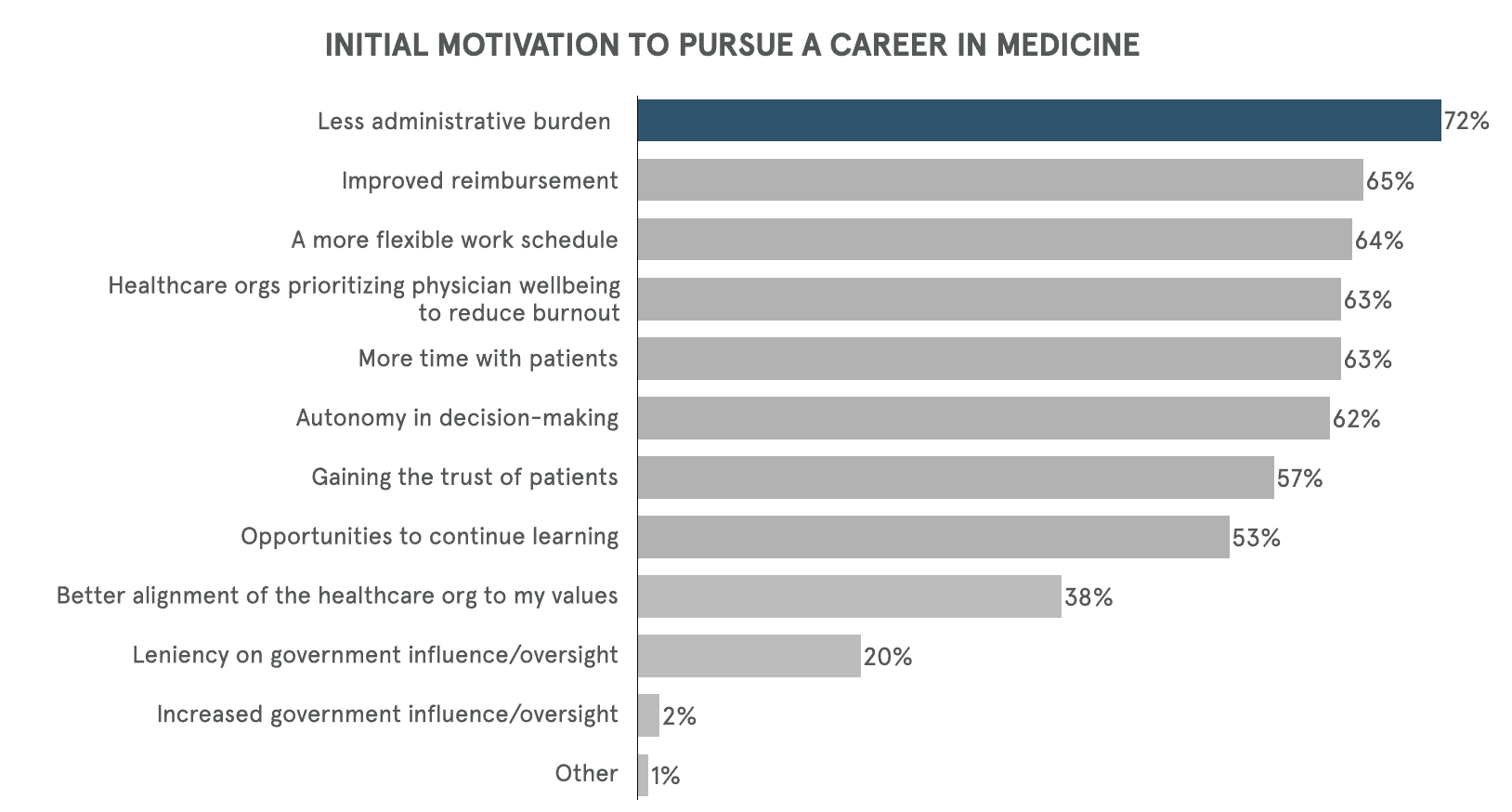
Over a third (38%) of young physicians surveyed said, “better alignment of the healthcare organization to my values” would be a requirement for how they want to practice medicine. This shift toward value-based medicine is a strong signal in value alignment becoming a critical factor in career decisions.

“I want to maintain my autonomy. That’s why I am a surgeon. I don’t want to be on the Henry Ford line and do this and that. I want to use my brain. I want autonomy to do what’s best and be able to take risks.” – Fellow, Surgery
There are potential issues, like dissatisfaction and burnout, when young physicians’ values don’t match those of their institutions. This desire for alignment extends beyond clinical work to encompass cultural and ethical practices.
Young physicians’ desire and commitment to practicing value-based medicine may be the momentum the healthcare ecosystem needs to continue an authentic pursuit of realizing value-based care.
In the Health 2035 Report published by LINUS and HSBC, we hypothesized that ideological immigrations — migrations driven by beliefs — will draw new literal and figurative borders that are made of communities with shared views and beliefs. In some medical communities, doctors and patients are moving to regions with healthcare practices and policies in line with their own ideological, health-related beliefs.
As a generation of doctors who lived, studied, and practiced through a pandemic — they are going to be looking for institutional and government support to better prepare for the next one. There’s an opportunity for institutions to demonstrate a stronger commitment to core values that align with their beliefs around equity, inclusivity, and work-life balance. Data shows that supporting these values of young physicians leads to better, more patient-centric care — a core tenant of realizing value-based care.
“Passion never drives the policies that are made. It’s easy to throw in the towel when issues get too challenging or impractical.” – Young Physician
Whether that manifests in policy reform for healthcare organizations to embrace core values of young physicians or incentives that demonstrate a strong commitment, young physicians’ expectations for institutions to demonstrate value-based medicine may change the dialogue and raise the bar for healthcare organizations to heed their call.
Young physicians feel strongly about the impact of early interventions. They consider them to be key drivers that will make the most positive impact on the delivery of care in healthcare in 2035, along with:
“If more people could wear a Fitbit or Apple Watch, it would provide more data for a mass education to self-triage in the emergency room.” – Dr. Shirlene Obuobi, Cardiology Fellow – Chicago Medical Center
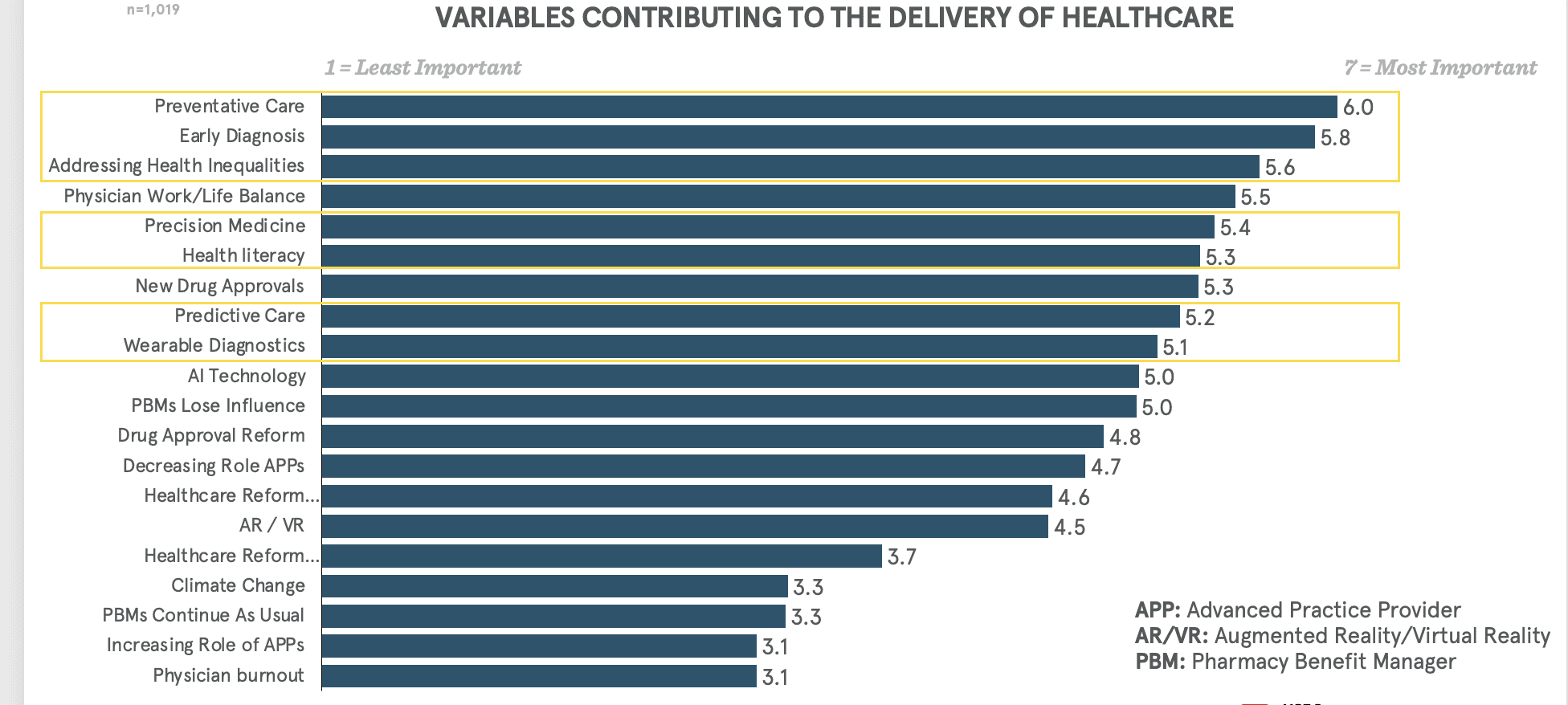
Systemic embracing of early interventions creates significant potential realignment of incentives for all the actors within the healthcare ecosystem, leading to creation of healthier populations and new forms of connection between physicians and their patients, and change the role of physicians in their communities.
The next generation of physicians are attuned to the advantages of preventative care and will continually encourage their patient interactions to move upstream.
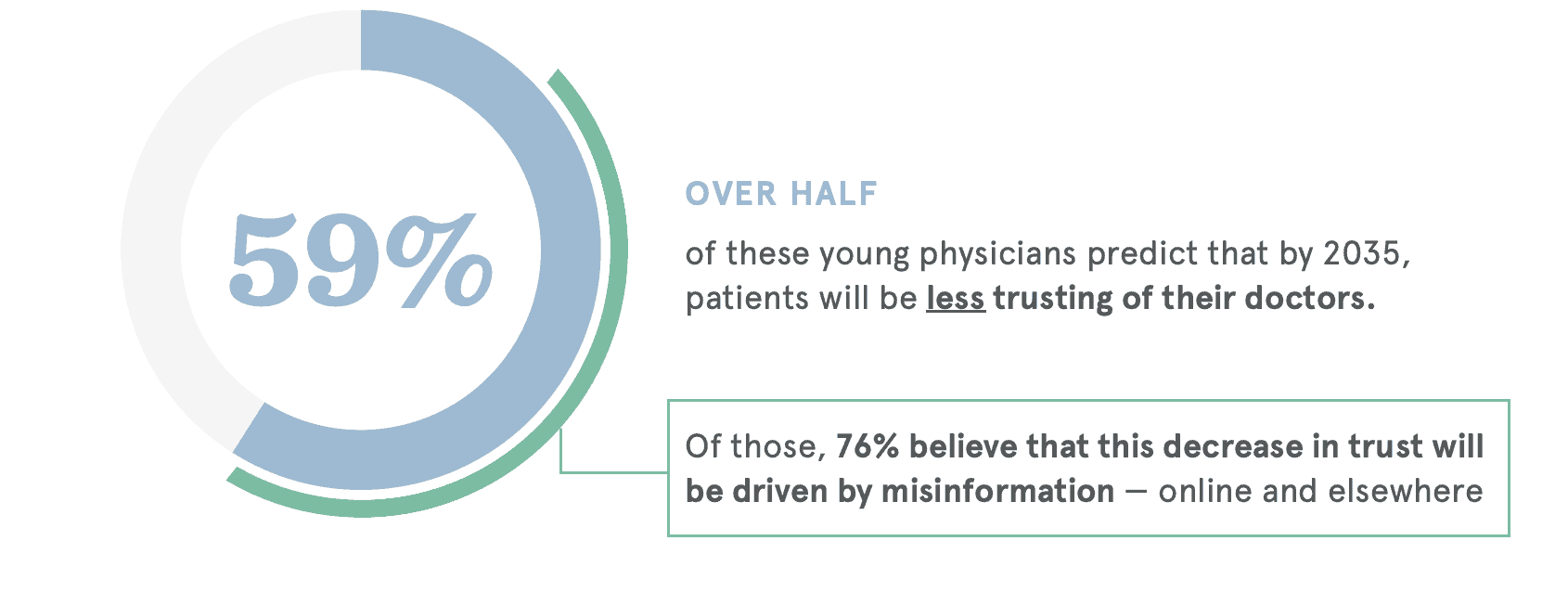
Trust is significantly eroding between both patients and physicians. Well over half (59%) of young physicians predict that in 2035, patients will be less trusting of their doctors. On the other hand, physicians also express a lack of trust in patients.
“I want to have a dialogue with my patients. I want to be friendly and let them know that I truly care. This builds more trust in the physicians and creates an open environment for patients to ask questions and have a deeper understanding of their health.” – Medical Student
The success of personal connections relies heavily on trust, which is increasingly challenged by misinformation. By 2035, young physicians project misinformation to be their top challenge.
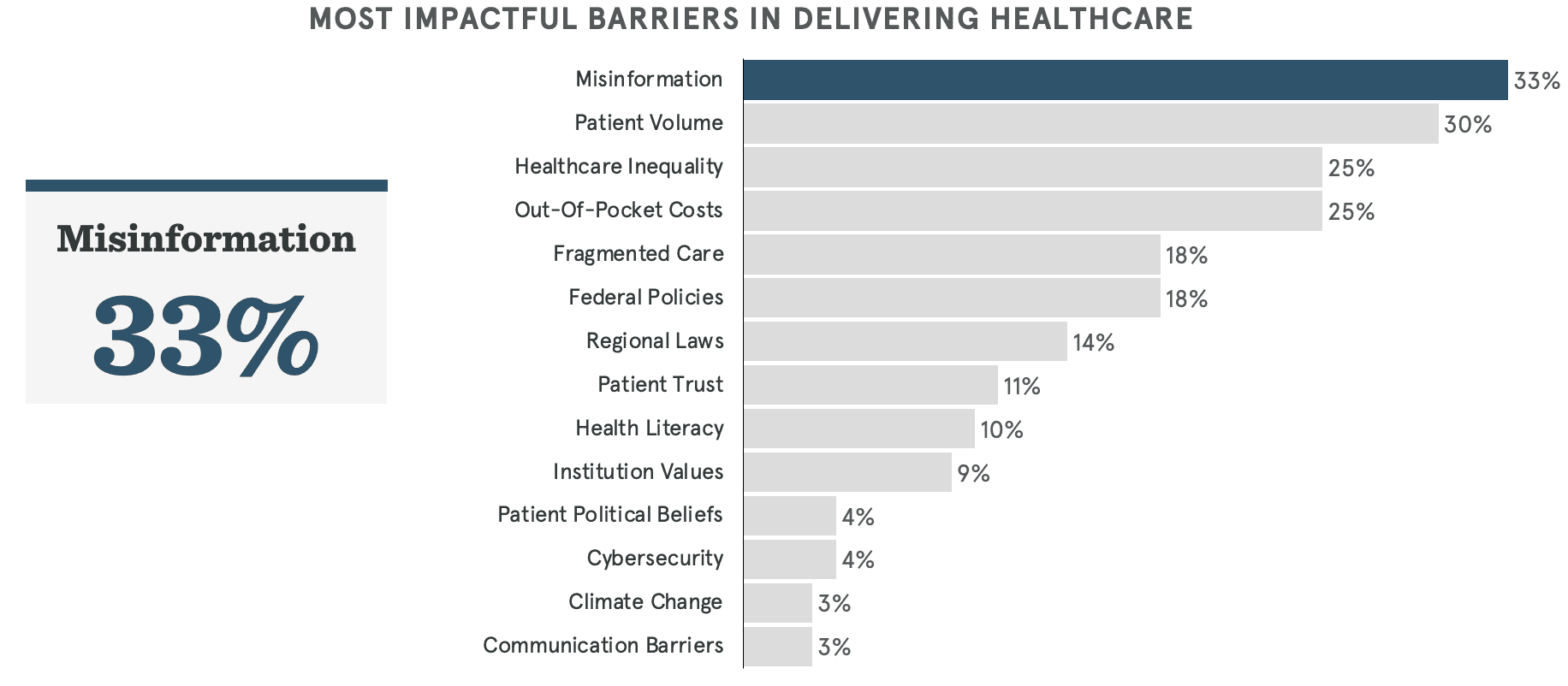
Of those who predict patients will trust them less, 76% of young physicians believe that this lack of confidence in them will be driven by misinformation — online and elsewhere.
“Social media is making pediatrics a whole lot harder. People are hesitant to believe doctors as they can find false information on the web and are too quick to believe it. People are wary about anything medicinal.” – Resident Physician, Pediatrics
Notably, medical students and physicians between the ages of 21-25 are most concerned with gaining the trust of their patients compared to those young physicians currently practicing. Nearly 70% of medical students selected “gaining the trust of patients” as a requirement for how they want to practice medicine. This suggests a potential focal point — establishing trust — for how the next generation of physicians will practice.
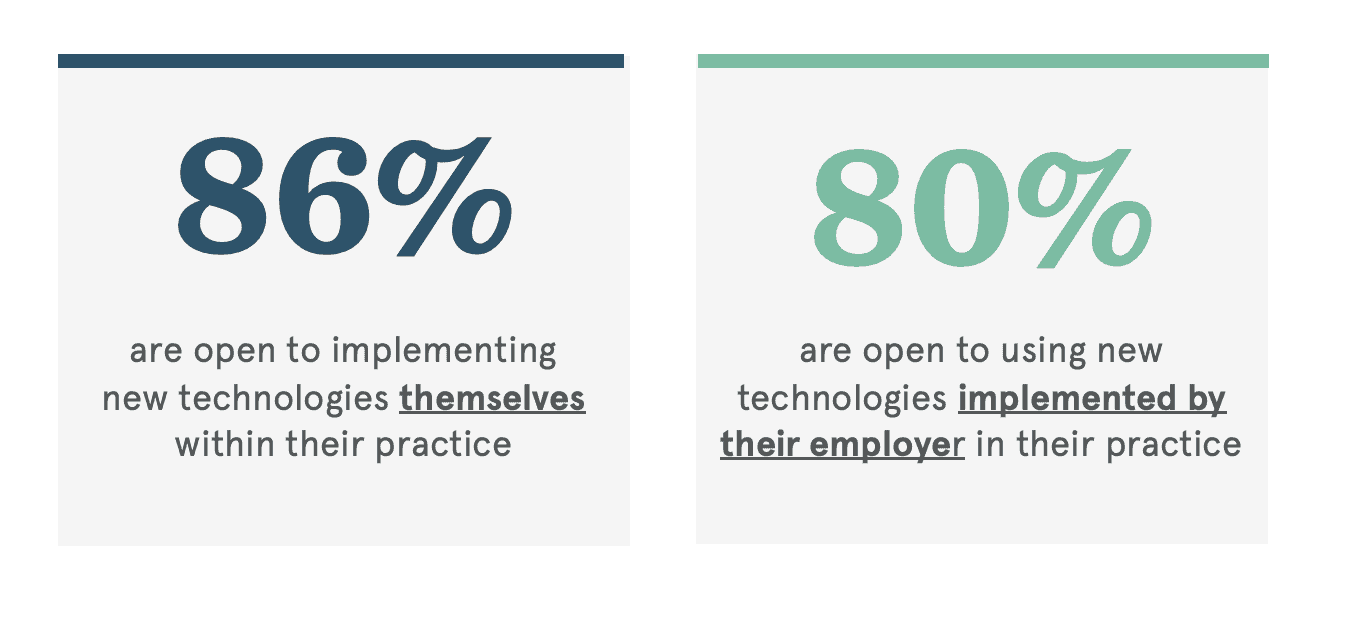
Nearly 90% of young physicians are open to implementing new technologies themselves within their practice, and another 80% are open to using new technologies provided by their employer.
“Technology is here to stay, and it is on us to figure out how to use it best. We need to be able to synthesize data faster, allowing us to spend more time making the connections with our patients and their health.” – Young Physician
Young physicians see more potential in AI for clinical decision-making, as opposed to helping with patient relationships.
By 2035, young physicians expect AI to change the way they practice. Around two-thirds of young physicians predict that the integration of artificial intelligence in the medical field will change how they engage with patients. This is over 60 percentage points higher than the second-most mentioned technology, telemedicine, indicating that this is a significant concern for young physicians.
This may signal their prediction and their desires to relegate AI’s role in their practice as one that is objective and administrative.
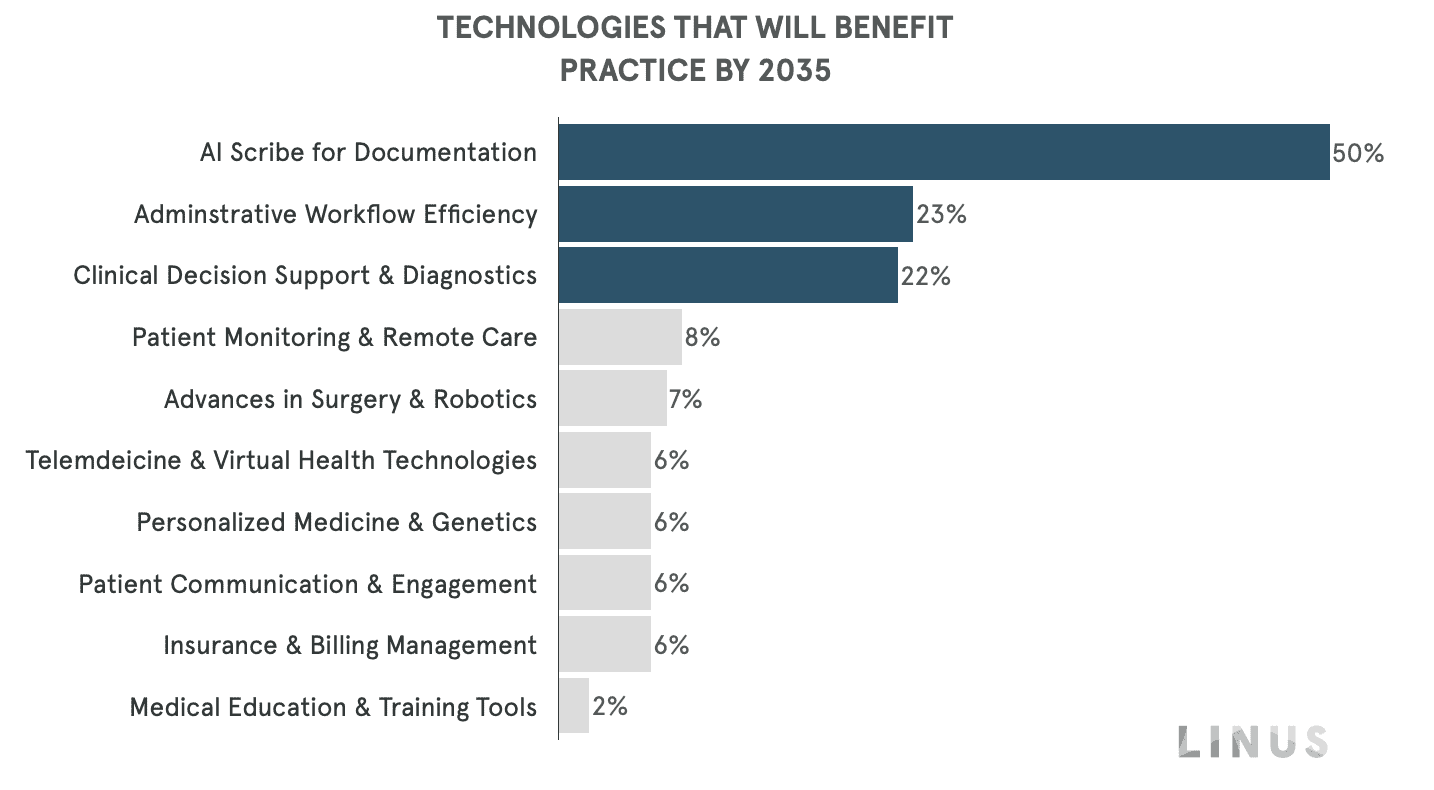
Half of respondents see the most useful tool for AI is as a scribe for documentation (50%), followed by administrative and workflow efficiencies (23%), and diagnostics and clinical decision support (22%). This presents an opportunity for AI to not only serve the overburdened and understaffed medical team, but can also step in as an advocate for patients — bridging a communication gap without impeding in the personal connections young physicians take pride in.
While young physicians self-identify as eager early technology adopters, the pace of technology innovation in healthcare may limit the true potential of the role technology may play in 2035.
The relationship between medical device or pharmaceutical companies and young physicians could have a significant, positive impact in how the healthcare ecosystem approaches clinical trials in the future. Young physicians are increasingly interested in shaping the future of healthcare through involvement in clinical trials and collaboration with medical device and pharmaceutical companies.
A significant percentage (24%) want to participate in designing and conducting clinical trials, and even more (70%) seek “educational relationships” with industry representatives to learn about new medicines and receive samples. With a generation of doctors that are highly invested in participating in the evolution of care through technology, this could lead to a pioneering moment in drug development that brings practical application and strong voices into the process.

There’s also notable interest — over ⅓ of young physicians — in serving on or attending advisory boards and providing guidance, particularly among dermatologists (51%) and radiologists (64%) who are significantly more likely to want to attend an advisory board meeting.
This represents a shift from past physician involvement in clinical trials, where only 3% of practicing physicians were involved in the roughly 74,000 registered clinical trials in the United States. Developments in health care during the past 10 years help make it easier for office-based clinicians to participate in these clinical trials. This presents an opportunity for the healthcare ecosystem to engage young physicians in the development and refinement of new technologies and therapies.
With a majority of young physicians (nearly 90%) open to implementing new technologies themselves within their practice, there’s an opportunity to bring young physicians into advisory boards for new devices and new therapies that address practical challenges and align with current medical practices and beliefs.
Their openness to implementing new technologies in their own practices further emphasizes their potential impact on the future of healthcare innovation.
Young physicians expect that the increasing responsibilities of healthcare providers like physician assistants and nurse practitioners will have a more negative impact than positive, as evidenced by a significant majority expressing concern over its potential negative impact by 2035.
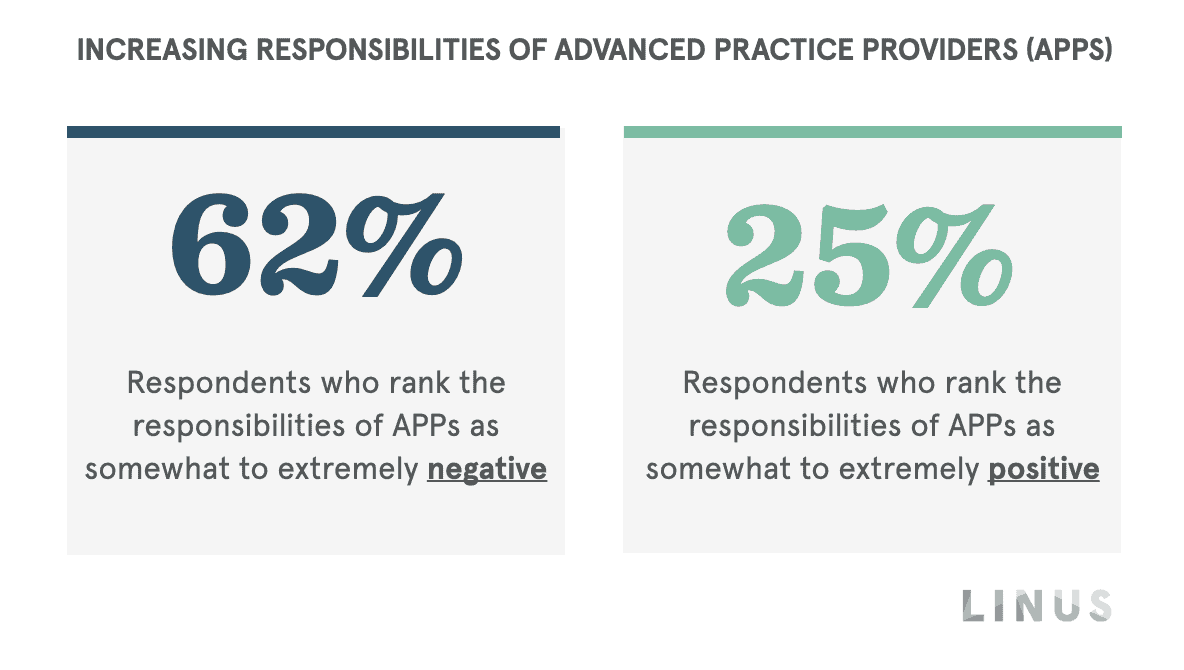
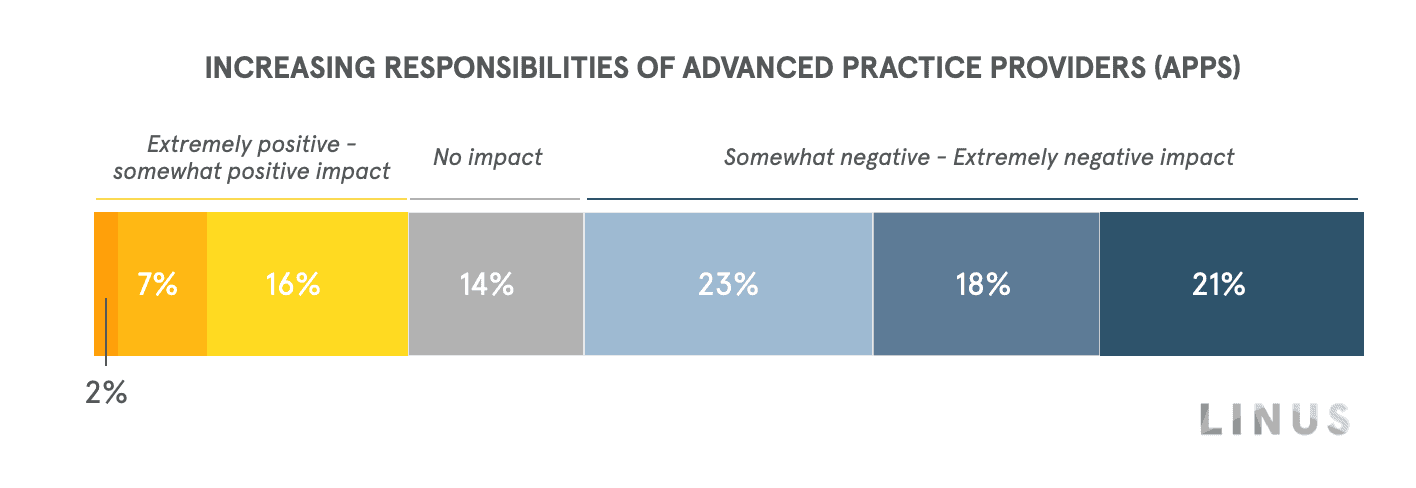
This apprehension may be largely due to the perceived risk of poorly-trained practitioners being pushed into service due to the oversized demand for healthcare organizations to address staffing shortages and burnout, potentially jeopardizing patient care. Programs that may circumvent traditional education curriculums to meet those demands may be doing more of a disservice than advantage by increasing the demand on under-prepared practitioners and how it may negatively affect patient care in the US.
“There are so many factors holding doctors back from utilizing their full degrees. Mid-level providers are excellent and can definitely be helpful but we need to define the scope in terms of what they can do more.” – Resident Physician, Pediatrics
This sentiment underscores a fundamental shift in healthcare decision-making, where the traditional physician-centric model is evolving, prompting young physicians to raise a “red flag”.
The successful adoption of the diversification and evolution of a patient’s care team requires cross-sector collaboration to deliver healthcare. Leveraging advanced technology for immersive educational training is one way young physicians hypothesize could have an extremely positive contribution to the delivery of healthcare in 2035.
While acknowledging the need for care-team diversification, young physicians are advocating for technology-enabled, educational training (like AR/VR) over fast-track programs that might compromise patient safety.
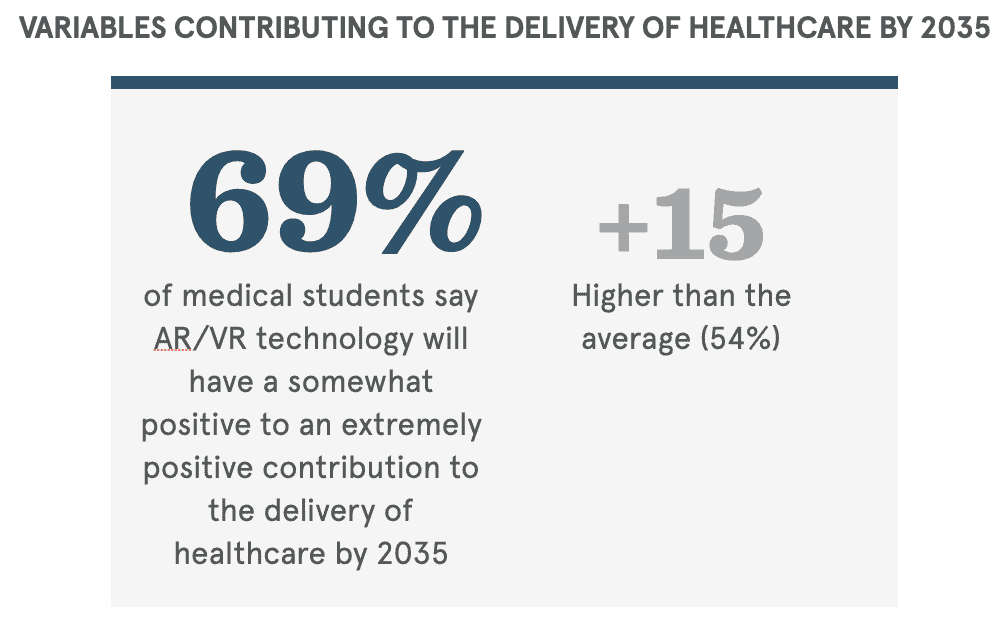
This highlights a critical tension: The need to address workforce shortages while maintaining rigorous standards and embracing technological advancements in medical education.
As leaders, we need to do everything we can to protect the human-centric delivery of care. Young physicians are deeply motivated by the personal connections with their patients and want to do the best thing for their health. With waning trust in both directions of the physician-patient relationship, such personal connection is at risk. This doesn’t mean we should forget technology. We must embrace it and use it as accelerators in clinical decision making and delivery of care. The future of care is here, and young physicians are ready for it.